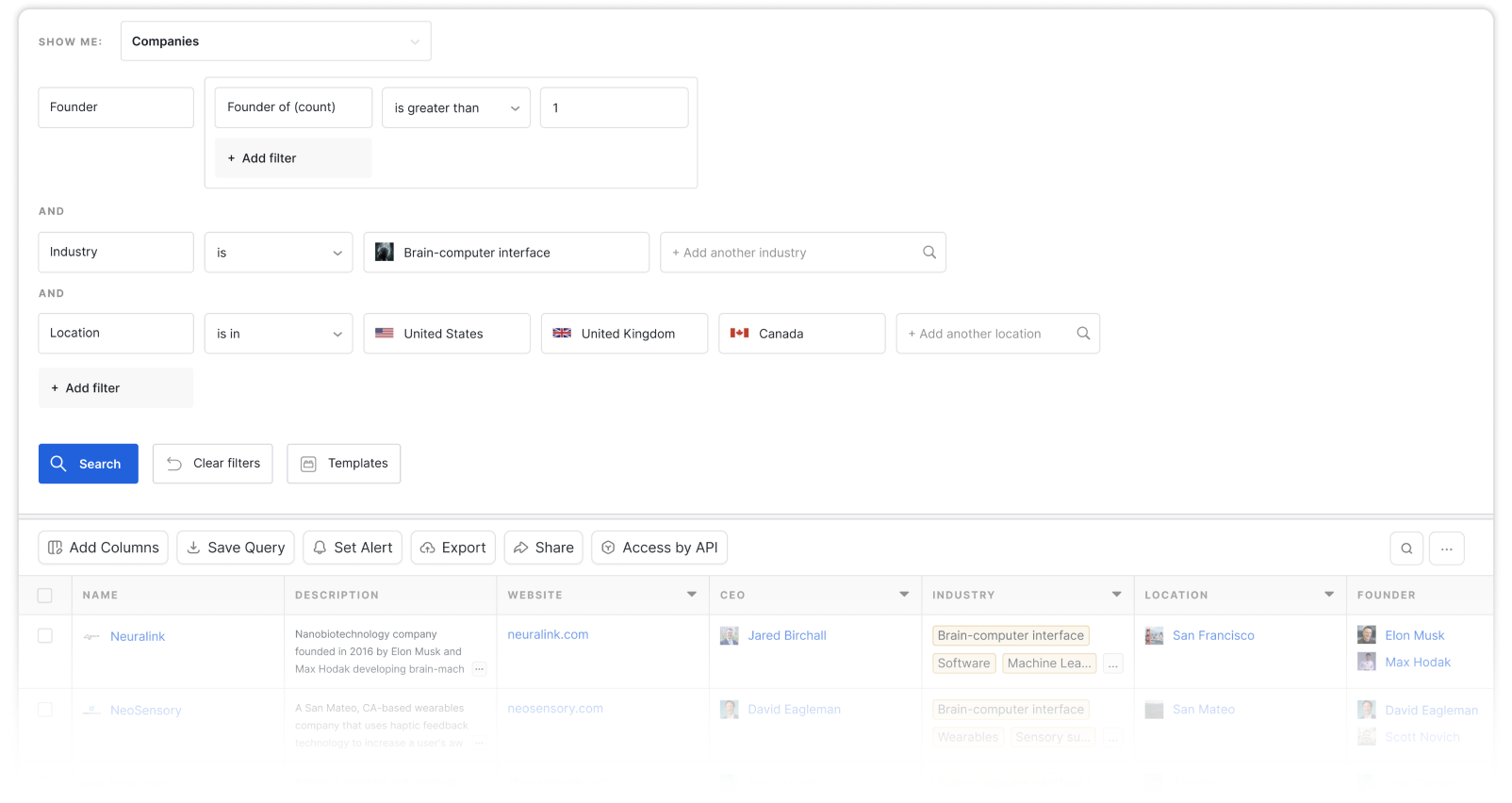
Industry attributes
Other attributes
The microbiome is the sum of microbes, including bacteria, archaea, viruses, microbial eukaryotes and fungi, and their genomic elements and interactions in their niches. Distinct microbiomes can be found on and in the body of an organism or in the environment. The NIH Common Fund Human Microbiome Project (HMP) is generating resources to facilitate characterization of the human microbiota for further understanding of how the microbiome impacts human health and disease. The Earth Microbiome Project aims to characterize all microbial life on earth and understand microbial ecology in different biomes and habitats.
The field of microbiomics, in which all microorganisms in a community or microbiota are analysed together, uses high-throughput DNA sequencing and RNA sequencing technologies and bioinformatics. Sample DNA is amplified and sequenced and compared to microbial genomic databases to find out the identities and diversity of microbes. Mass spectrometry and nuclear magnetic resonance spectroscopy are used to analyze metabolic interactions between the microbiome and host.
The human microbiome is the collection of all the microorganisms living in association with the human body. These communities consist of a variety of microorganisms including eukaryotes, archaea, bacteria, fungi and viruses. Distinct distributions of microbial taxa make up regional microbiomes in different habitats within the human body including skin microbiome, gut microbiome, lung microbiome, oral microbiome, placenta microbiome and vaginal microbiome.
Non-pathogenic organisms affect human health and homeostasis through a variety of mechanisms including metabolism of nutrients and drugs, synthesis of vitamins, defense against pathogens, host bile acid secondary processing, modulation of the immune system and modulation of behavior through production of neuroactive compounds.
The skin microbiome makeup depends on age, gender, ethnicity, climate, UV exposure and lifestyle factors. The oily, sebaceous gland sites are predominantly inhabited by Propionibacterium species. Staphylococcus species are found in moist microenvironments. Malassezia is a common fungal flora on human skin.
Atopic dermatitis (AD), also known as eczema, is associated with dysfunction of the epidermal barrier and linked to Staphylococcus aureus overgrowth and a concomitant decrease in Staphylococcus epidermidis. S. aureus overgrowth is associated with severity of AD and increased allergen sensitization. Antimicrobials that target S. aureus have been shown to reduces AD severity. In contrast, a study on the skin microbiome of infants with AD showed an absence of S. aureus suggesting that colonization with S. aureus may not always predate clinical AD. Members of healthy skin microbiota which are often reduced in AD patients include Propionibacterium, Streptococcus, Acinetobacter, Corynebacterium, Prevotella and Proteobacteria. The fungi, Malassezia are found on healthy skin but increased colonization in AD may contribute to disease pathogenesis.
S. aureus can contribute to disruption of the epidermal barrier. An impaired skin barrier increases the exposure of the immune system to microbial components and result in a progressive cycle of inflammatory responses. It has been suggested that allergen exposure can increase reactivity to S. aureus and visa versa.
Several connections between skin and gut microbiota dysbiosis have been found. AD has been associated with changes in gut microbiota, with lower levels of Bifidobacterium in the gut than controls. Some studies have shown alterations in gut microbiota composition preceding AD, such as colonization with C. difficile and low Bacteriodetes diversity. In children with AD, whole-metagenome analysis showed depletion of mucin-degrading bacteria such as Akkermansia muciniphila, Ruminococcus gnavus and Lachnospiraceae, bacteria that can influence the immune development.
Dog exposure at birth was found to be associated with reduced risk of AD in early life, suggesting exposure to more microbial components in the environment may be protective. Increased risk of AD is associated with use of antibiotics in the first 2 years of life. Intestinal inflammation at 2 months of age is associated with an increased risk of AD and asthma by 6 years of age.
Most human studies on neonates suggest that contact with maternal and environmental microbes establishes early colonizers of the infant intestine. Vaginally delivered babies have microbial communities in their intestine dominated by Lactobacillus spp. And Bifidobacterium spp., which are similarly found in the vaginal canal of their mothers. Babies delivered by cesarean section are colonized predominantly by skin microbes with Staphylococcus being the predominant genus. The neonatal gut provides a selective environment, allowing some organisms to colonize and inhibiting others.
Differences between the gut microbes in in babies delivered vaginally versus by caesarean could also be due to confounding factors such as antibiotic administration, labor onset, maternal body weight, maternal diet, gestational age and breastfeeding frequency/duration. Research suggests that differences in intestinal microbe composition between vaginally delivered and caesarean delivered babies resolve after solid foods are introduced. However, the gut microbiome plays an important role in the development of the immune system early in life, which can impact neurodevelopment and risk of metabolic and immune-related diseases later in life.
Receptors on the cell surface of immune cells, such as toll-like receptors (TLRs) recognize pathogen-associated molecular patterns (PAMPs) from microorganisms from components such as lipopolysaccharides (LPS), peptidoglycans, lipoteichoic acid, flagellin and muramyldipeptide. Constituents of gram-negative bacteria such as LPS have been found to help trigger low-grade inflammation and insulin resistance through interaction between receptors in the innate immune system and gut microbes. Increased circulating LPS is a condition called metabolic endotoxaemia that has been found in genetic models of diet-induced obesity and diabetes as well as in humans.
The gut barrier, that separates the intestinal lumen from the inside of the body, is controlled by communication between gut microbes and the host immune system. Loss of immune tolerance is associated with inflammation of the bowel.
The Canadian Healthy Infant Longitudinal Development (CHILD) study found a lower abundance of bacteria of the genera Lachnospira, Veillonella, Faecalibacterium and Rothia in the gut was associated with asthma later in life and linked mechanistically to reduced faecal short-chain fatty acids (SCFAs). High levels of SCFAs in early life have been shown to be protective against sensitization and asthma later in life. In as US study on a birth cohort, changes in relative abundance of certain microbes in the gut of neonates increased risk of multisensitized atopy and asthma. The children at increased risk had increased pro-inflammatory metabolites including those that induce IL-4 production in CD4+ T cells and decrease abundance of regulatory T cells (Tregs).
Colonization of airways with Streptococcus, Moraxella or Haemophilus in first 2 months of life has been associated with virus-induced acute respiratory infections and asthma later on. Reduced risk of wheezing at 2 years old was associated with increased abundance of Lactobacillus species at 2 months of age during acute respiratory infection caused by respiratory syncytial virus (RSV).
One Health is a new term but is also a long recognized concept that recognizes connections between the health of people, animals and the environment and it is an approach used by the Centers for Disease Control and Protection (CDC). The One Health approach has also been applied to microbiome relationships in humans, animals and the environment. The environmental microbiome and the microbiome of animals can affect the human microbiome, impacting human health.